|
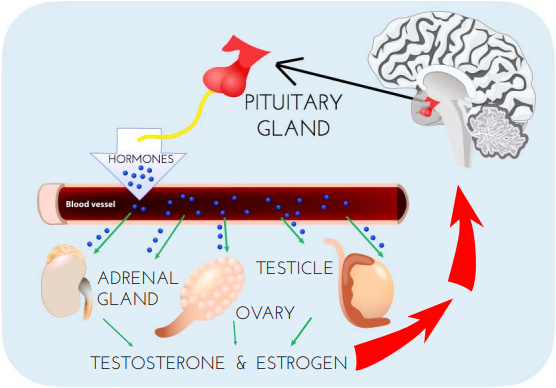
(Image credit: Dana Foundation - Illustration by Elizabeth A. Weaver II) Male Contraceptive Initiative provides funding and advocacy support for the development of non-hormonal, reversible forms of male contraception. But what does “non-hormonal” mean? How do these methods differ from “hormonal” contraceptives? In this post, we share a primer on the difference between hormonal and non-hormonal contraception. Hormonal Contraception Hormonal contraceptives are birth control methods that impact the endocrine system, which is the system of the body that creates the regulatory substances (i.e., hormones) that are transported in tissue fluids (e.g., blood) and stimulate specific cells or tissues into action. In other, simpler terms, hormones allow cells to effectively “talk” to each other. Hormones are part of the function of virtually every cell and organ in the body. They control our moods, growth and development, metabolism, and more. If your endocrine system is not functioning properly, it can lead to issues related to stress management, puberty, and even the ability to get pregnant. The latter of which explains why hormones can be developed to impact the endocrine system for contraceptive purposes. There are two main types of hormonal contraceptive formulations:
It should be noted that, while hormonal contraception is primarily used for the prevention of pregnancy, it can and is also prescribed for the treatment of polycystic ovary syndrome (PCOS), menstrual disorders such as dysmenorrhea and menorrhagia, and hirsutism. Non-hormonal Contraception Contraceptives classified as “non-hormonal” are exactly that: methods that do not affect a person's hormones. Some common types on non-hormonal contraceptives include:
These methods tend to have fewer side effects (e.g., headaches, nausea, depression, yeast infections, reduced sexual desire, etc.) than their hormonal counterparts and are not negatively impacted by interactions with other medical therapies (e.g., antibiotics). However, some of these methods, such as withdrawal and the rhythm method, have low efficacy, and might not provide reliable contraception. Non-hormonal pharmaceutical products are currently in development for both men and women. These products will allow users greater flexibility in delivery options (e.g. pills, injectables) similar to current hormonal contraceptive offerings, without the potential drawbacks associated with hormonal method use. These products are designed to prevent pregnancy using a more targeted approach, focusing on inhibiting the activity or developmental pathway of a specific cell (e.g. sperm cells). Due to the specific action of these products, the chance of “off-target” effects is reduced, ultimately resulting in few or no side-effects. Male Contraceptive Initiative focuses specifically on the development of non-hormonal contraceptive options for men. We feel that the time is right to take advantage of new technological developments and provide reproductive autonomy for all in a form that is reliable, safe, and reversible. Nuts & Bolts: Hormonal vs. Non-hormonal Contraception To learn more about, please visit our series of posts about male reproduction and contraception: Key terms Cervical mucus - fluid or gel-like discharge from the cervix. Throughout a woman's menstrual cycle, the thickness and amount of cervical mucus changes due to fluctuating hormone levels. Cervix - the narrow passage forming the lower end of the uterus. Conception - the process of becoming pregnant involving fertilization or implantation or both. Contraception - the deliberate use of artificial methods or other techniques to prevent pregnancy as a consequence of sexual intercourse. Contraceptives - devices or drugs designed to prevent pregnancy. Diaphragm - A birth control device made of soft silicone and shaped like a shallow cup that covers the cervix to prevent pregnancy. Dysmenorrhea - throbbing or cramping pains in the lower abdomen. Ejaculation - the action of ejecting semen from the body. Endocrine System - a chemical messenger system consisting of hormones, the group of glands of an organism that secrete those hormones directly into the circulatory system to regulate the function of distant target organs, and the feedback loops which modulate hormone release so that homeostasis is maintained. Estrogen - any of a group of steroid hormones which promote the development and maintenance of female characteristics of the body. Hirsutism - abnormal growth of hair on a person's face and body, especially on a woman. Hormone - a regulatory substance produced in an organism and transported in tissue fluids such as blood or sap to stimulate specific cells or tissues into action. Intrauterine Device (IUD) - a small, often T-shaped birth control device that is inserted into the uterus to prevent pregnancy. Menorrhagia - medical term for menstrual periods with abnormally heavy or prolonged bleeding. Ovulation - the release of an egg during menstruation in females. Polycystic ovary syndrome (PCOS) - a condition that affects how the function of ovaries. Progestogen/Progestin - a natural or synthetic steroid hormone, such as progesterone, that maintains pregnancy and prevents further ovulation during pregnancy. Progesterone - a steroid hormone released by the corpus luteum that stimulates the uterus to prepare for pregnancy. Puberty - the period during which adolescents reach sexual maturity and become capable of reproduction. Spermicide - a substance that kills spermatozoa, used as a contraceptive. Sponge - contraceptive device that prevents sperm from entering the cervix and also contains spermicide. For additional terminology related to male contraception and the male reproductive system, please visit our glossary: Sources/References Susan Scott Ricci; Terri Kyle (2009). "Common Reproductive Issues". Contraception. Lippincott Williams & Wilkins. p. 119. "Noncontraceptive Benefits of Birth Control Pills". Reproductivefacts.org. The American Society for Reproductive Medicine. Retrieved 5 May 2013. Paladine, Heather (2003). "What's New In Contraception". The Female Patient. Retrieved 2009-08-30. "Progestin-only Contraceptives". Hall Health Primary Care Center. University of Wisconsin-Seattle. 2007-02-11. "Combined Estrogen-Progestogen Contraceptives" (PDF). IARC Monographs on the Evaluation of Carcinogenic Risks to Humans. International Agency for Research on Cancer. 91. 2007. IARC Working Group on the Evaluation of Carcinogenic Risks to Humans (1999). "Hormonal contraceptives, progestogens only". Hormonal contraception and post-menopausal hormonal therapy; IARC monographs on the evaluation of carcinogenic risks to humans, Volume 72. Lyon: IARC Press. pp. 339–397. ISBN 92-832-1272-X. Nelson, Anita L.; Cwiak, Carrie (2011). "Combined oral contraceptives (COCs)". In Hatcher, Robert A.; Trussell, James; Nelson, Anita L.; Cates, Willard Jr.; Kowal, Deborah; Policar, Michael S. (eds.). Contraceptive technology (20th revised ed.). New York: Ardent Media. pp. 249–341. ISBN 978-1-59708-004-0. ISSN 0091-9721. OCLC 781956734. pp. 257–258. Speroff, Leon; Darney, Philip D. (2011). "Oral contraception". A clinical guide for contraception (5th ed.). Philadelphia: Lippincott Williams & Wilkins. pp. 19–152. ISBN 978-1-60831-610-6. Levin, Ellis R.; Hammes, Stephen R. (2011). "Estrogens and progestins". In Brunton, Laurence L.; Chabner, Bruce A.; Knollmann, Björn C. (eds.). Goodman & Gilman's pharmacological basis of therapeutics (12th ed.). New York: McGraw-Hill Medical. pp. 1163–1194. ISBN 978-0-07-162442-8. Glasier, Anna (2010). "Contraception". In Jameson, J. Larry; De Groot, Leslie J. (eds.). Endocrinology (6th ed.). Philadelphia: Saunders Elsevier. pp. 2417–2427. ISBN 978-1-4160-5583-9. Perone N (1993). "The history of steroidal contraceptive development: the progestins". Perspect Biol Med. 36 (3): 347–62. doi:10.1353/pbm.1993.0054. PMID 8506121. S2CID 46312750. "Hirsutism and Polycystic Ovary Syndrome". American Society for Reproductive Medicine. Retrieved 5 May 2013. "Hirsutism and Polycystic Ovary Syndrome (PCOS)". American Society for Reproductive Medicine. Retrieved 5 May 2013. Callahan, Tamara; Caughey, Aaron B. (2013). Blueprints Obstetrics and Gynecology. Lippincott Williams & Wilkins. p. 320. ISBN 9781451117028. "ParaGard (copper IUD)". Drugs.com. 7 September 2019. Retrieved 3 December 2019. "IUD (intrauterine device)". Contraception guide. NHS Choices. Retrieved 2 March 2014. the intrauterine device, or IUD (sometimes called a coil) Ortiz, ME; Croxatto HB (June 2007). "Copper-T intrauterine device and levonorgestrel intrauterine system: biological bases of their mechanism of action". Contraception. 75 (6): S16–30. "Definition of Birth control". MedicineNet. Archived from the original on August 6, 2012. Retrieved August 9, 2012. Hanson SJ, Burke AE (2010). "Fertility control: contraception, sterilization, and abortion". In Hurt KJ, Guile MW, Bienstock JL, Fox HE, Wallach EE (eds.). The Johns Hopkins manual of gynecology and obstetrics (4th ed.). Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins. pp. 382–395. ISBN 978-1-60547-433-5. World Health Organization (WHO). "Family planning". Health topics. World Health Organization (WHO). Archived from the original on March 18, 2016. Retrieved March 28, 2016. Grimes DA, Gallo MF, Grigorieva V, Nanda K, Schulz KF (October 2004). "Fertility awareness-based methods for contraception". The Cochrane Database of Systematic Reviews (4): CD004860. For additional publications related to male contraception and the male reproductive system, please visit our publications page: Comments are closed.
|
Categories
All
Archives
June 2024
|
|
|
Donate to Male Contraceptive InitiativeYour generous donation makes a difference!
|
© Male Contraceptive Initiative. All rights reserved.

 RSS Feed
RSS Feed
